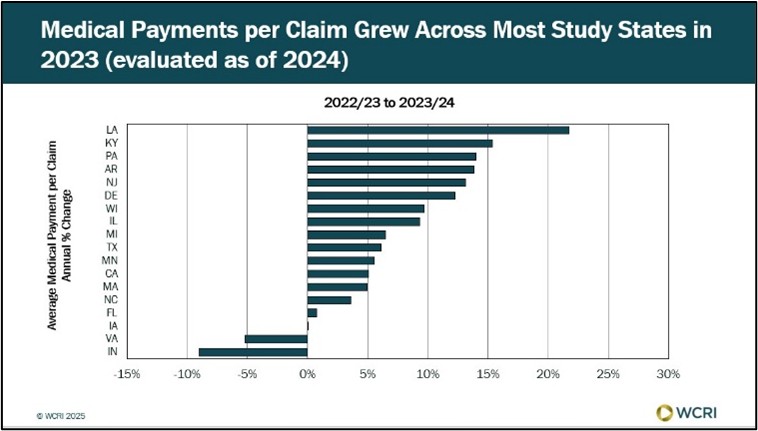
Waltham, MA, October 9, 2025 — After a period of relative stability post-COVID, new studies from the Workers Compensation Research Institute (WCRI) show that medical costs per claim have begun to rise.
“Medical payments per claim remained relatively stable, but recently, they started increasing, fueled by an increase in medical utilization, medical prices, and updates to state fee schedules,” said Sebastian Negrusa, WCRI vice president of research.
The studies, CompScope™ Medical Benchmarks, 2025 Edition, examine medical payments, prices, and utilization overall, by provider, and by type of service across 18 states, showing how these metrics have changed over time. Key findings from a few of the individual studies include the following:
- California: After several years of stable medical payments since 2018, California recently saw a 5% increase in medical payments per claim, with increases in payments per claim for several nonhospital services, including physical medicine services, contributing to that growth.
- Delaware: Medical payments per claim grew 7% per year between 2021 and 2023, driven by price increases in professional and hospital outpatient services. These trends align with Delaware’s fee schedule, which is adjusted based on the Consumer Price Index for All Urban Consumers (CPI-U).
- Pennsylvania: Medical payments per claim for care provided to injured workers increased 14 percent in 2023 after years of decreases, reflecting, in part, larger recent annual updates to the state’s medical fee schedule, which is tied to the statewide average weekly wage.
- Wisconsin: Medical payments per claim grew 6% per year from 2021 to 2023 after years of small changes. Wisconsin, which has had some of the highest medical payments per claim among the study states, recently passed legislation introducing a medical fee schedule for hospital services.
The results reflect the experience of non-COVID-19 claims through March 2024. The 18 states in the study—Arkansas, California, Delaware, Florida, Illinois, Indiana, Iowa, Kentucky, Louisiana, Massachusetts, Michigan, Minnesota, New Jersey, North Carolina, Pennsylvania, Texas, Virginia, and Wisconsin—represent about 60% of all workers’ compensation benefit payments nationwide.
The studies are free for members and available to nonmembers for a fee.
 Back to News
Back to News